Physiology of Pain
Pain is a universal experience that can greatly impact our daily lives. Whether it's a stubbed toe or a chronic condition, understanding the physiology of pain is essential for effective management and relief. In this article, we will delve into the intricate mechanisms behind pain perception and explore the factors that influence its intensity. So, let's dive in and unravel the physiology of pain.
Pain serves as a vital warning signal for our bodies, alerting us to potential harm or injury. It prompts us to take appropriate action to protect ourselves and seek relief. However, the experience of pain goes beyond a simple response to external stimuli. It involves a complex interplay of physiological processes and psychological factors.
Bradykinin in the physiology of pain
Prostaglandins in the physiology of pain
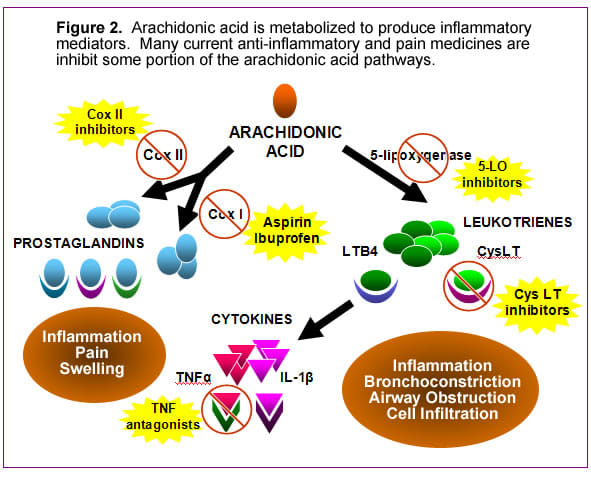
Arachidonic acid produces some of the chemicals involved in the physiology of pain such as, prostaglandins....Motrin is a basic pain med that blocks this acid.
Chemicals involved in the physiology of pain.
What is Pain?
Pain can be defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage. It is a subjective phenomenon, varying in intensity and quality between individuals. Pain can be categorized into three main types:
Types of Pain
a) Acute Pain: Acute pain is short-lived and usually arises from an injury, surgery, or illness. It serves as a warning sign that something is wrong and requires immediate attention.
b) Chronic Pain: Chronic pain persists for an extended period, typically longer than three months. It can result from conditions such as arthritis, fibromyalgia, or nerve damage. Chronic pain can significantly impact a person's quality of life and often requires multidimensional management.
c) Neuropathic Pain: Neuropathic pain arises from direct damage or dysfunction of the nervous system. It is characterized by shooting, burning, or tingling sensations and can be caused by conditions like diabetic neuropathy or postherpetic neuralgia.
The Nervous System
To understand the physiology of pain, we must first explore the intricate network of the nervous system, which plays a central role in pain perception.
Nociceptors
Nociceptors are specialized nerve endings that detect and respond to painful stimuli. They are found throughout the body, particularly in the skin, joints, and organs. When activated by mechanical, thermal, or chemical stimuli, nociceptors send electrical signals to the brain, signaling the presence of potential harm.
Pain Pathway
Once nociceptors detect a painful stimulus, they transmit electrical impulses along nerve fibers to the spinal cord. From there, the signals ascend to the brain, specifically the thalamus and cerebral cortex, where pain is perceived and processed. This complex pathway involves various neurotransmitters and receptors, which modulate the intensity and quality of the pain experience.
Spinal cord in physiology of pain
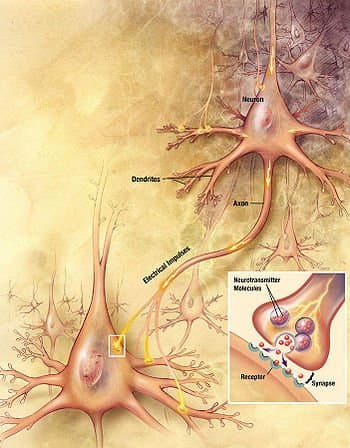
Glutamate and aspartate are released by A-delta fibers and somatostatin and substance P are released by C-fibers in the synapses of the spinal cord. Which are thought to enhance transmission of the pain signal.
Perspectives of physiology of pain Part 1
A-delta and C-fibers in the physiology of pain
Pain can be further classified into different categories based on its underlying physiological mechanisms. Understanding these categories can provide insights into targeted treatment approaches.
Sensory Pain
Sensory pain, also known as nociceptive pain, arises from the activation of nociceptors in response to harmful stimuli. It is characterized by a well-defined location and a sharp or aching quality. Sensory pain can be further divided into somatic and visceral pain.
Inflammatory Pain
Inflammatory pain occurs as a result of tissue damage or inflammation. It is associated with redness, swelling, and increased sensitivity in the affected area. Inflammatory pain involves the release of chemical mediators, such as prostaglandins, that sensitize nociceptors and contribute to the overall pain experience.
Neuropathic Pain
Neuropathic pain stems from damage or dysfunction of the nervous system itself. It often presents as a shooting, burning, or electric shock-like sensation. Nerve injuries, compression, or diseases like multiple sclerosis can lead to neuropathic pain. It involves aberrant nerve signaling and altered processing within the central nervous system.
Pain Perception
The perception of pain is a highly subjective and multifaceted process. It is influenced by various factors, including psychological, genetic, and environmental aspects.
Dorsal horn of spinal cord
Dorsal horn of spinal cord is the relay station to and from the higher levels of the Central nervous system.
Perspectives of physiology of pain part 2
Factors Influencing Pain
Psychological Factors
Psychological factors, such as anxiety, depression, and stress, can significantly influence the perception and experience of pain. Negative emotions can amplify pain signals, while positive emotions and relaxation techniques may help alleviate pain.
Genetic Factors
Genetics also play a role in pain perception. Certain gene variations can affect the sensitivity to pain or the efficacy of pain medications. Understanding genetic factors can aid in personalized pain management strategies.
Environmental Factors
Environmental factors, such as social support, cultural beliefs, and previous experiences, can shape the individual's pain experience. The context in which pain occurs can influence its interpretation and coping mechanisms.
Management of Pain
Effectively managing pain requires a multidimensional approach tailored to the individual's specific needs. Treatment options range from medications to non-pharmacological interventions.
Medications
Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, and anticonvulsants can be used to alleviate pain. However, their use should be carefully monitored to mitigate the risk of side effects and addiction.
Non-Pharmacological Approaches
Non-pharmacological interventions, including physical therapy, acupuncture, cognitive-behavioral therapy, and relaxation techniques, can complement medication-based treatments. These approaches aim to enhance overall well-being and provide relief from pain.
Understanding the physiology of pain is crucial for effective pain management. Pain is a complex phenomenon that involves the nervous system, subjective perception, and various influencing factors. By unraveling the intricacies of pain, we can develop targeted strategies to alleviate suffering and improve the quality of life for individuals experiencing pain.
Physiology of pain: Acute pain
Acute pain doesn't last very long, but must be assessed properly to make sure it is not pointing to a new disease process.
Physiology of pain: Chronic Pain
Somatic pain
Visceral pain
Neuropathic pain
FAQs
Q1: How long does acute pain typically last?
A1: Acute pain is usually short-lived and lasts until the underlying cause of the pain is resolved or healed.
Q2: Can chronic pain be completely cured?
A2: Chronic pain is often a complex condition that requires multidimensional management. While complete cure may not always be possible, effective management can significantly improve quality of life.
Q3: Are there any natural remedies for pain relief?
A3: Some natural remedies, such as herbal supplements, hot and cold therapy, and meditation, may provide temporary pain relief. However, it's essential to consult with a healthcare professional before trying any alternative treatments.
Q4: Can genetics determine pain tolerance?
A4: Genetics can influence an individual's pain tolerance to some extent. Certain gene variations may make someone more or less sensitive to pain.
Q5: How can psychological techniques help with pain management?
A5: Psychological techniques, such as cognitive-behavioral therapy and relaxation exercises, can help individuals develop coping strategies, manage stress, and reduce the perception of pain.
Remember, pain management should always be done under the guidance of healthcare professionals who can provide personalized advice and treatment options based on individual needs.
Sources
- International Association for the Study of Pain (IASP) - www.iasp-pain.org
- National Institute of Neurological Disorders and Stroke (NINDS) - www.ninds.nih.gov
- Mayo Clinic - www.mayoclinic.org
- American Academy of Pain Medicine (AAPM) - www.painmed.org
Comments
hiit on June 07, 2012:
Really fantastic hub. "We must learn our limits. We are all something, but none of us are everything." by Blaise Pascal.
Ron from Fitness http://www.intervalstraining.net
hatry on September 28, 2011:
why pain increases heart rate?
FoFo on March 07, 2011:
what's the difference between referred pain and radiating pain?
manu on November 01, 2010:
hi...
In general, In acute pain incidence cases, In practical what is distribution of cases means how many suffers from visceral, somatic and neuropathic pain in Percentage (%)
If you have any information on this thing please send me on nipermanoj@rediffmail.com
Levi (author) from New Mexico on July 10, 2010:
Please feel free to ask any question that you may have.....or give me a thumbs up or down. Physiology of pain is the subject studied in order to treat pain. Questions, or comments definitely welcome.